1. What is the benefit of lung ultrasound?
In the past few years, lung ultrasound imaging has been used more and more clinically. From the traditional method of only judging the presence and amount of pleural effusion, it has revolutionized lung parenchyma imaging examination. We can diagnose the 5 most common severe causes of acute respiratory failure (pulmonary edema, pneumonia, pulmonary embolism, COPD, pneumothorax) in more than 90% of cases with a simple 3-5 minute lung ultrasound. The following is a brief introduction to the general process of lung ultrasonography.
2. How to choose an ultrasound probe?
The most commonly used probes for lung ultrasound are L10-5 (also called small organ probe, frequency range 5~10MHz linear array) and C5-2 (also called abdominal probe or large convex, 2~5MHz convex array), some scenarios can also Use P4-2 (also called cardiac probe, 2~4MHz phased array).
The traditional small organ probe L10-5 is easy to obtain a clear pleural line and observe the echo of the subpleural tissue. The rib can be used as a marker to observe the pleural line, which can be the first choice for pneumothorax assessment. The frequency of abdominal probes is moderate, and the pleural line can be observed more clearly while examining the entire chest. Phased array probes are easy to image through the intercostal space and have a deep detection depth. They are often used in the assessment of pleural effusions, but are not good at detecting pneumothorax and pleural space conditions.

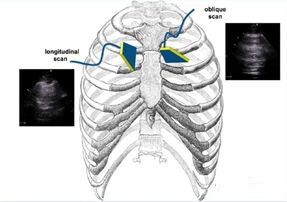
3. Which parts should be checked?
Lung ultrasonography is commonly used in the modified bedside lung ultrasonography (mBLUE) scheme or the two-lung 12-division scheme and the 8-division scheme. There are a total of 10 checkpoints on both sides of the lungs in the mBLUE scheme, which is suitable for situations requiring rapid inspection. The 12-zone scheme and the 8-zone scheme are to slide the ultrasound probe in each area for a more thorough scan.
The locations of each checkpoint in the mBLUE scheme are shown in the following figure:


| checking point | Location |
| blue dot | The point between the middle finger and the base of the ring finger on the side of the head |
| diaphragm point | Find the location of the diaphragm with the ultrasound probe in the midaxillary line |
| point M
|
The midpoint of the line connecting the upper blue point and the diaphragm point |
|
PLAPS point
|
The intersection of the extension line of point M and the line perpendicular to the posterior axillary line |
| back blue dot
|
The area between the subscapular angle and the spine |
The 12-division scheme is based on the patient's parasternal line, anterior axillary line, posterior axillary line, and paraspinal line to divide the thorax into 6 areas of anterior, lateral, and posterior chest wall, and each area is further divided into two areas, up and down, with a total of 12 areas. area. The eight-partition scheme does not include the four areas of the posterior chest wall, and is often used in the diagnosis and evaluation of ultrasonography for interstitial pulmonary syndrome. The specific scanning method is to start from the midline in each area, the central axis of the probe is completely perpendicular to the bony thorax (longitudinal plane), first slide laterally to the demarcation line, return to the midline, then slide medially to the demarcation line, and then return midline.

4. How to analyze ultrasound images?
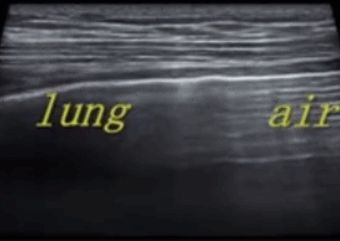
As we all know, air is the "enemy" of ultrasound, because ultrasound decays rapidly in air, and the presence of air in the lung makes it difficult to directly image the lung parenchyma. In a normally inflated lung, the only tissue that can be detected is the pleura, which appears on ultrasound as a horizontal hyperechoic line called the pleural line (the one closest to the soft tissue layer). In addition, there are parallel, repetitive hyperechoic horizontal line artifacts called A-lines below the pleural line. The presence of an A-line means that there is air below the pleural line, which can be normal lung air or free air in a pneumothorax.
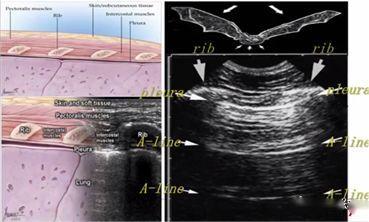
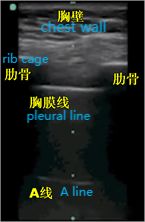
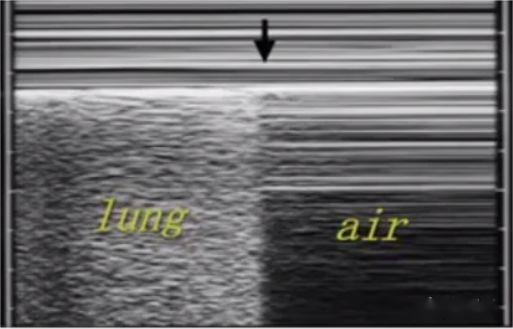
During lung ultrasonography, the pleural line is first located, unless there is a lot of subcutaneous emphysema, which is usually visible. In normal lungs, the visceral and parietal pleura may slide relative to each other with breathing, which is called lung sliding. As shown in the next two images, the upper image has lung sliding and the lower image has no lung sliding.
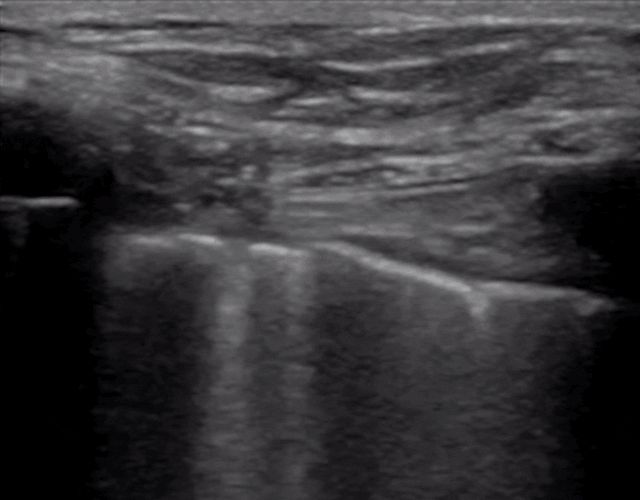
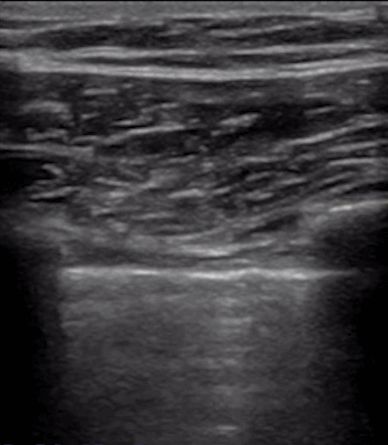

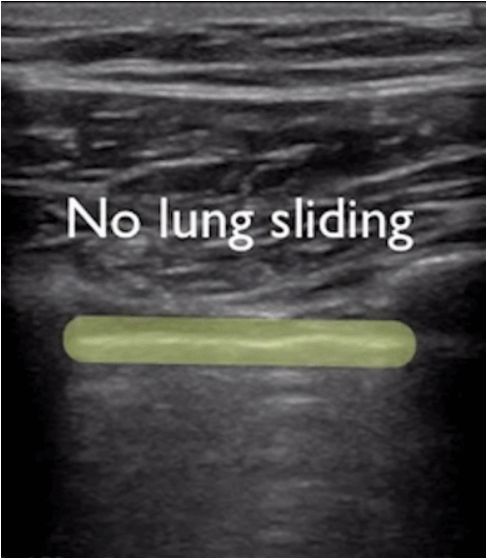
Generally, in patients with pneumothorax, or a large amount of pleural effusion that keeps the lungs away from the chest wall, the lung sliding sign will disappear. Or pneumonia consolidates the lungs, and adhesions appear between the lungs and the chest wall, which can also make the lung sliding sign disappear. Chronic inflammation produces fibrous tissue that reduces lung mobility, and thoracic drainage tubes cannot see lung sliding as in advanced COPD.
If the A line can be observed, it means that there is air below the pleural line, and the lung sliding sign disappears, it is likely to be a pneumothorax, and it is necessary to find a lung point for confirmation. The lung point is the transition point from no lung sliding to normal lung sliding in pneumothorax and is the gold standard for ultrasound diagnosis of pneumothorax.
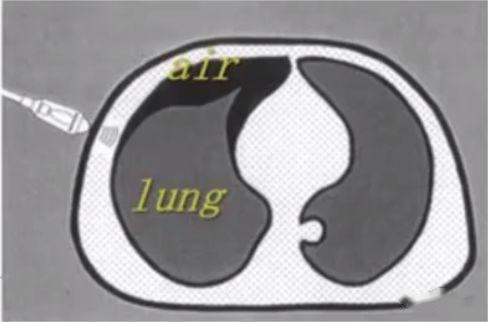
Multiple parallel lines formed by relatively fixed chest wall can be seen under M-mode ultrasound. In normal lung parenchyma images, due to lung sliding back and forth, sand-like echoes are formed underneath, which is called the beach sign. There is air below the pneumothorax, and there is no lung sliding, so multiple parallel lines are formed, which is called the barcode sign. The dividing point between the beach sign and the barcode sign is the lung point.
If the presence of A-lines is not visible in an ultrasound image, it means that some tissue structure in the lung has changed, allowing it to transmit ultrasound. Artifacts such as A-lines disappear when the original pleural space is filled by tissue such as blood, fluid, infection, contusion caused by clotted blood, or a tumor. Then you need to pay attention to the problem of line B. The B-line, also known as the "comet tail" sign, is a laser beam-like hyperechoic strip emitting vertically from the pleural line (visceral pleura), reaching the bottom of the screen without attenuation. It masks the A-line and moves with the breath. For example, in the picture below, we can't see the existence of the A line, but instead of the B line.
Don't worry if you get several B-lines on an ultrasound image, 27% of normal people have localized B-lines in the 11-12 intercostal space (above the diaphragm). Under normal physiological conditions, less than 3 B lines are normal. But when you encounter a large number of diffuse B-lines, it is not normal, which is the performance of pulmonary edema.
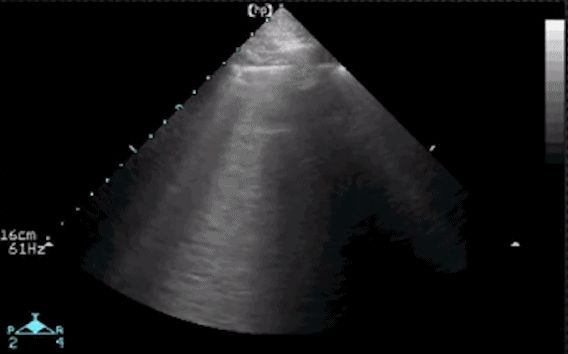
After observing the pleural line, A line or B line, let's talk about pleural effusion and lung consolidation. In the posterolateral area of the chest, pleural effusion and lung consolidation can be better assessed. The image below is an ultrasound image examined at the point of the diaphragm. The black anechoic area is the pleural effusion, which is located in the pleural cavity above the diaphragm.


So how do you differentiate between pleural effusion and hemorrhage? Fibrous exudate can sometimes be seen in hemopleural effusion, while the effusion is usually a black homogeneous anechoic area, sometimes divided into small chambers, and floating objects of varying echo intensity can be seen around .
Ultrasound can visually assess the majority (90%) of patients with lung consolidation, the most basic definition of which is loss of ventilation. The amazing thing about using ultrasound to diagnose lung consolidation is that when a patient's lungs are consolidated, the ultrasound can pass through the deep-thoracic areas of the lung where consolidation occurs. Lung tissue was hypoechoic with wedge-shaped and indistinct borders. Sometimes you may also see the air bronchus sign, which is hyperechoic and moves with breathing. The sonographic image that has specific diagnostic significance for lung consolidation in ultrasound is the liver tissue-like sign, which is a solid tissue-like echo similar to liver parenchyma that appears after the alveoli are filled with exudate. As shown in the figure below, this is an ultrasound image of lung consolidation caused by pneumonia. In the ultrasound image, some areas can be seen as hypoechoic, which looks a bit like the liver, and no A can be seen.

Under normal circumstances, the lungs are filled with air, and color Doppler ultrasound cannot see anything, but when the lungs are consolidated, especially when there is pneumonia near the blood vessels, even blood flow images in the lungs can be seen, as follows as shown in the figure.

The sound of identifying pneumonia is the basic skill of lung ultrasound. It is necessary to move back and forth between the ribs to carefully check whether there is a hypoechoic area, whether there is air bronchus sign, whether there is a liver tissue-like sign, and whether there is normal A-line or not. Lung ultrasound image.
5. How to decide the results of ultrasonography?
Through a simple ultrasound scan (mBLUE scheme or twelve-zone scheme), the characteristic data can be classified, and the severe cause of acute respiratory failure can be determined. Quickly completing the diagnosis can relieve the patient's dyspnea more quickly and reduce the use of complex examinations such as CT and UCG. These characteristic data include: lung sliding, A performance (A lines on both thoracic cavities), B performance (B lines appearing in both thoracic cavities, and there are no less than 3 B lines or adjacent B lines are adhered), A /B appearance (A appearance on one side of the pleura, B appearance on the other side), lung point, lung consolidation, and pleural effusion.
Post time: Dec-20-2022