History of central venous access
1. 1929: German surgeon Werner Forssmann placed a urinary catheter from the left anterior cubital vein, and confirmed with X-ray that the catheter entered the right atrium
2. 1950: Central venous catheters are mass-produced as a new option for central access
3. 1952: Aubaniac proposed subclavian vein puncture, Wilson subsequently proposed CVC catheterization based on the subclavian vein
4. 1953: Sven-Ivar Seldinger proposed to replace the hard needle with a metal guide wire guide catheter for peripheral venipuncture, and the Seldinger technique became a revolutionary technology for central venous catheter placement
5. 1956: Forssmann, Cournand, Richards won the Nobel Prize in Medicine for their contribution to cardiac catheterization
6. 1968: First report in English of internal jugular venous access for central venous pressure monitoring
7. 1970: The concept of tunnel catheter was first proposed
8. 1978: Venous Doppler locator for internal jugular vein body surface marking
9. 1982: The use of ultrasound to guide central venous access was first reported by Peters et al.
10. 1987: Wernecke et al first reported the use of ultrasound to detect pneumothorax
11. 2001: The Bureau of Health Research and Quality Evidence Reporting lists central venous access point-of-care ultrasound as one of 11 practices worthy of widespread promotion
12. 2008: American College of Emergency Physicians lists ultrasound-guided central venous access as a "core or primary emergency ultrasound application"
13.2017: Amir et al suggest that ultrasound can be used to confirm CVC location and exclude pneumothorax to save time and ensure accuracy
Definition of central venous access
1. CVC generally refers to the insertion of a catheter into the central vein through the internal jugular vein, subclavian vein and femoral vein, usually the tip of the catheter is located in the superior vena cava, inferior vena cava, caval-atrial junction, right atrium or brachiocephalic vein, among which the superior vena cava. Venous or cavity-atrial junction is preferred
2. Peripherally inserted central venous catheter is PICC
3. Central venous access is mainly used for:
a) Concentrated injection of vasopressin, inositol, etc.
b) Large-bore catheters for infusion of resuscitation fluids and blood products
c) Large bore catheter for renal replacement therapy or plasma exchange therapy
d) Parenteral nutrition management
e) Long-term antibiotic or chemotherapy drug treatment
f) Cooling catheter
g) Sheaths or catheters for other lines, such as pulmonary artery catheters, pacing wires and endovascular procedures or for cardiac interventional procedures, etc.
Basic principles of ultrasound-guided CVC placement
1.Assumptions of traditional CVC cannulation based on anatomical landmarks: expected vascular anatomy and patency of veins
2. Principles of Ultrasound Guidance
a) Anatomical variation: vein location, body surface anatomical markers themselves; ultrasound allows real-time visualization and assessment of vessels and adjacent anatomy
b) Vascular patency: Preoperative ultrasonography can detect thrombosis and stenosis in time (especially in critically ill patients with high incidence of deep vein thrombosis)
c) Confirmation of inserted vein and catheter tip positioning: real-time observation of guidewire entry into vein, brachiocephalic vein, inferior vena cava, right atrium or superior vena cava
d) Reduced complications: thrombosis, cardiac tamponade, arterial puncture, hemothorax, pneumothorax
Probe and Equipment Selection
1. Equipment features: 2D image is the basis, color Doppler and pulsed Doppler can distinguish between arteries and veins, medical record management as part of patient medical records, sterile probe cover/couplant ensures sterile isolation
2. Probe selection:
a) Penetration: The internal jugular and femoral veins are usually 1-4 cm deep under the skin, and the subclavian vein needs 4-7 cm
b) suitable resolution and adjustable focus
c) Small size probe: 2~4cm wide, easy to observe the long and short axes of blood vessels, easy to place the probe and needle
d) 7~12MHz small linear array is generally used; small convex under the clavicle, children's hockey stick probe
Short-axis method and long-axis method
The relationship between the probe and the needle determines whether it is in-plane or out-of-plane
1. The needle tip cannot be seen during the operation, and the position of the needle tip needs to be determined by dynamically swinging the probe; advantages: short learning curve, better observation of perivascular tissue, and easy placement of the probe for fat people and short necks;
2. The complete needle body and needle tip can be seen during the operation; it is challenging to keep the blood vessels and needles in the ultrasound imaging plane at all times
static and dynamic
1. Static method, ultrasound is only used for preoperative assessment and selection of needle insertion points
2. Dynamic method: real-time ultrasound-guided puncture
3. Body surface marking method < static method < dynamic method
Ultrasound-guided CVC puncture and catheterization
1. Preoperative preparation
a) Patient information registration to keep chart records
b) Scan the site to be punctured to confirm vascular anatomy and patency, and determine the surgical plan
c) Adjust image gain, depth, etc. to get the best image state
d) Place the ultrasound equipment to ensure that the puncture point, probe, screen and line of sight are collinear
2. Intraoperative skills
a) Physiological saline is used on the skin surface instead of the couplant to prevent the couplant from entering the human body
b) The non-dominant hand holds the probe lightly and leans lightly against the patient for stabilization
c) Keep your eyes fixed on the ultrasound screen, and feel the pressure changes sent back by the needle with your hands (feeling of failure)
d) Introducing the guide wire: The author recommends that at least 5 cm of the guide wire be placed in the central venous vessel (ie, the guide wire should be at least 15 cm from the needle seat); Need to enter 20~30cm, but the guide wire enters so deep, it is easy to cause arrhythmia
e) Confirmation of the position of the guide wire: Scan along the short axis and then the long axis of the blood vessel from the distal end, and track the position of the guide wire. For example, when the internal jugular vein is punctured, it is necessary to confirm that the guide wire enters the brachiocephalic vein.
f) Make a small incision with a scalpel before dilation, the dilator goes through all the tissue in front of the blood vessel, but avoid puncturing the blood vessel
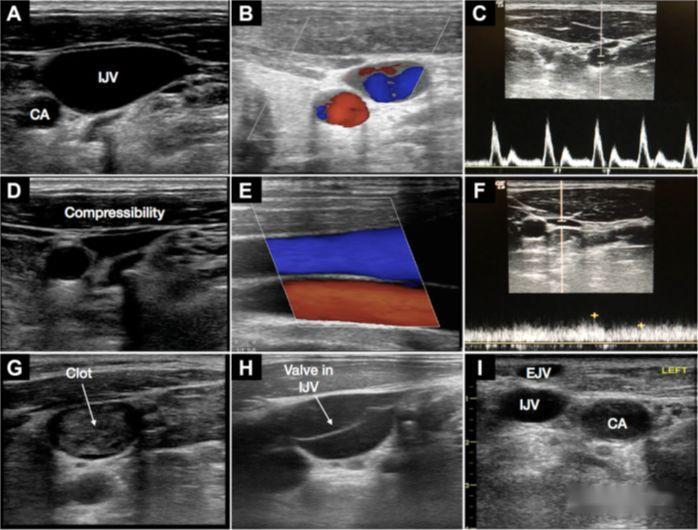
3. Internal Jugular Vein Cannulation Trap
a) The relationship between the carotid artery and the internal jugular vein: Anatomically, the internal jugular vein is generally located on the outside of the artery. During short-axis scanning, because the neck is round, scanning at different positions forms different angles, and overlapping veins and arteries may occur. Phenomenon.
b) Selection of the needle entry point: the proximal tube diameter is large, but it is closer to the lung, and the risk of pneumothorax is high; it is recommended to scan to confirm that the blood vessel at the needle entry point is 1~2cm deep from the skin
c) Scan the entire internal jugular vein in advance, assess the anatomy and patency of the blood vessel, avoid thrombus and stenosis at the puncture point and separate it from the carotid artery
d) Avoid carotid artery puncture: Before vasodilation, the puncture point and the position of the guide wire need to be confirmed in the long and short axis views. For safety reasons, the long axis image of the guide wire needs to be seen in the brachiocephalic vein.
e) Turning the head: The traditional marking puncture method recommends turning the head to highlight the sternocleidomastoid muscle marking and exposing and fixing the internal jugular vein, but turning the head 30 degrees may cause the internal jugular vein and carotid artery to overlap by more than 54%, and ultrasound-guided puncture is not possible. It is recommended to turn
4.Subclavian vein catheterization
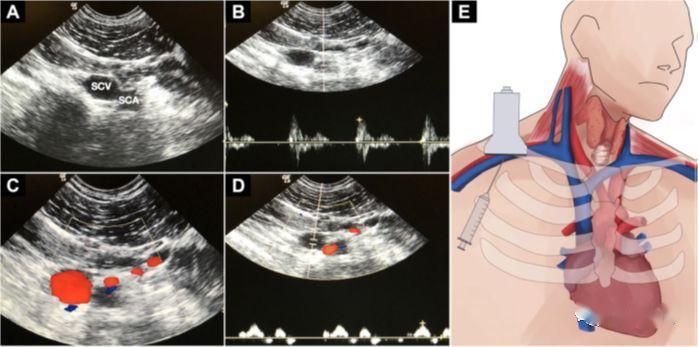
a) It should be noted that the ultrasound scan of the subclavian vein is somewhat difficult
b) Advantages: The anatomical position of the vein is relatively reliable, which is convenient for in-plane puncture
c) Skills: The probe is placed along the clavicle in the fossa below it, showing the short-axis view, and the probe slowly slides down the middle; technically, the axillary vein is punctured here; turn the probe 90 degrees to show the long-axis view of the blood vessel , the probe is slightly tilted towards the head; after the probe is stabilized, the needle is punctured from the center of the probe side, and the needle is inserted under the real-time ultrasound guidance
d) Recently, small microconvex puncture with slightly lower frequency has been used to guide, and the probe is smaller and can see deeper
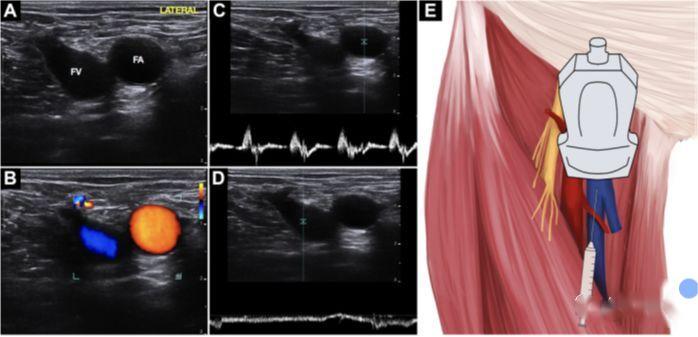
5. Femoral vein catheterization
a) Advantages: Keep away from respiratory tract and monitoring equipment, no risk of pneumothorax and hemothorax
b) There is not much literature on ultrasound-guided puncture. Some people think that it is very reliable to puncture the body surface with obvious markers, but ultrasound is inefficient. Ultrasound guidance is very suitable for FV anatomical variation and cardiac arrest.
c) Frog leg posture reduces the overlap of the top of the FV with the FA, raises the head and extends the legs outward to widen the venous lumen
d) The technique is the same as for internal jugular vein puncture
Cardiac ultrasound guide wire positioning
1. TEE cardiac ultrasound has the most accurate tip positioning, but it is damaging and cannot be used routinely
2. Contrast enhancement method: use the microbubbles in the shaking normal saline as a contrast agent, and enter the right atrium within 2 seconds after laminar flow ejection from the catheter tip
3. Requires extensive experience in cardiac ultrasound scanning, but can be verified in real time, attractive
Lung ultrasound scan to rule out pneumothorax
1. Ultrasound-guided central venous puncture not only reduces the incidence of pneumothorax, but also has high sensitivity and specificity for detection of pneumothorax (higher than chest X-ray)
2. It is recommended to integrate it into the postoperative confirmation process, which can quickly and accurately check at the bedside. If it is integrated with the previous section of cardiac ultrasound, it is expected to shorten the waiting time for catheter use.
3. Lung ultrasound: (external supplementary information, for reference only)
Normal lung image:
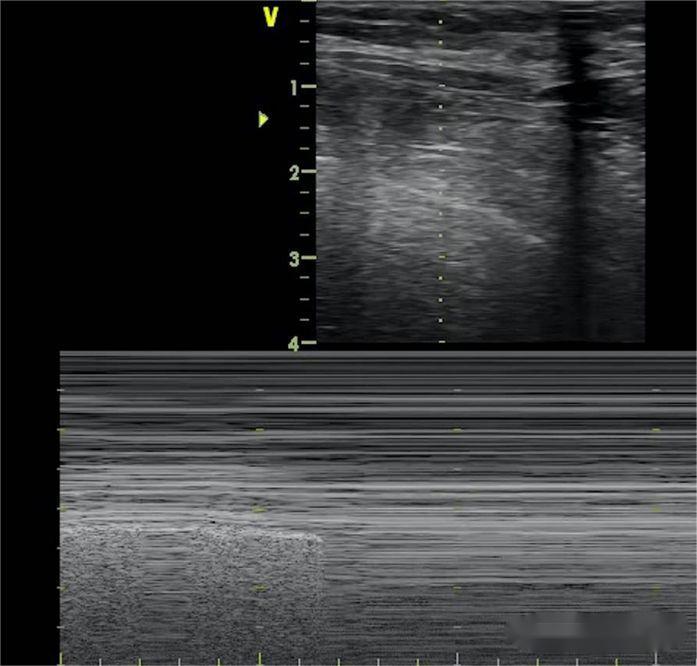
Line A: The pleural hyperechoic line that slides with breathing, followed by multiple lines parallel to it, equidistant, and attenuated with depth, that is, lung sliding
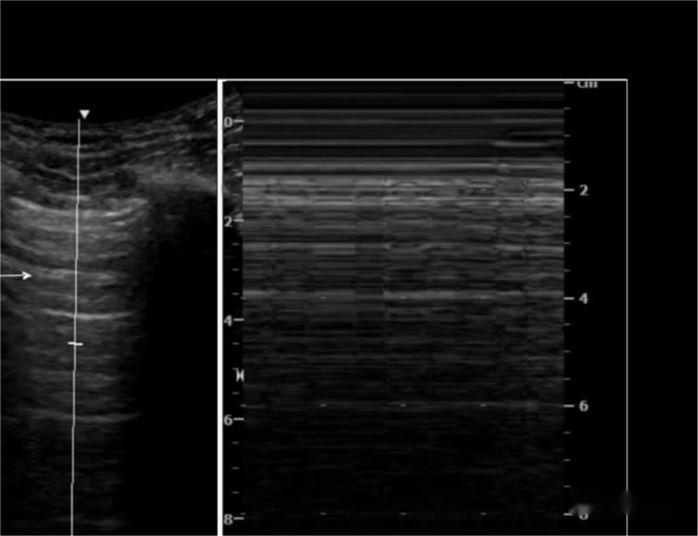
M-ultrasound showed that the hyperechoic line reciprocating in the direction of the probe with respiration was like the sea, and the pectoral mold line was sand-like, that is, the beach sign

In some normal people, the last intercostal space above the diaphragm can detect less than 3 laser beam-like images originating from the pectoral mold line, extending vertically at the bottom of the screen, and reciprocating with breathing—B line
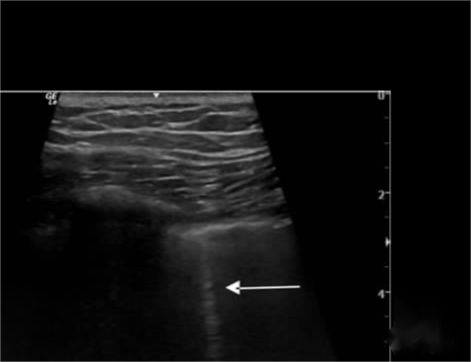
Pneumothorax Image:
The B line disappears, the lung sliding disappears, and the beach sign is replaced by the barcode sign. In addition, the lung point sign is used to determine the extent of pneumothorax, and the lung point appears where the beach sign and the barcode sign alternately appear.
Ultrasound-Guided CVC Training
1. Lack of consensus on training and certification standards
2. The perception that blind insertion techniques are lost in learning ultrasound techniques exists; however, as ultrasound techniques become more widespread, the choice between patient safety and maintenance of techniques that may be less likely to be used must be considered
3. Assessment of clinical competence should be scored by observing clinical practice rather than relying on the number of procedures
in conclusion
The key to efficient and safe ultrasound-guided CVC is awareness of the pitfalls and limitations of this technique in addition to proper training
Post time: Nov-26-2022